Age, morbidity, or something else? A residual approach using microdata to measure the impact of technological progress on health care expenditure
Laudicella M., Li Donni P., Olsen K.R., Gyrd-Hansen D., 2022 – Health Economics
Technological progress and change in medical practice are important drivers of public health expenditure growth in many high-income countries, accounting for 40-70% of total health expenditure growth. Moreover, they are the engine of an impressive success in reducing mortality and increasing life expectancy associated with several diseases, allowing individuals to participate in society’s progress for longer. Understanding the rise in healthcare expenditures (HCE) in high-income countries is a central focus for future health policy.
In a recent article, “Age, morbidity, or something else? A residual approach using microdata to measure the impact of technological progress on health care expenditure”, published in Health Economics, Mauro Laudicella, Paolo Li Donni, Kim Rose Olsen and Dorte Gyrd-Hansen investigate whether changes in healthcare spending can be primarily attributed to aging populations and morbidity, or other factors, particularly technological advancements and changes in medical practices, play a crucial role.
The primary objective of the study is to measure the extent to which non-demographic factors contribute to increases in HCE over time. This inquiry arises from the observed phenomenon that healthcare spending growth often surpasses demographic changes. Moreover, the authors decompose the residual increase (RI) in HCE into components that can be attributed to (a) delayed time to death (TTD)—individuals living longer following health shocks—and (b) increased intensity of resource use – i.e. more comprehensive service demands from individuals.
The research exploits a residual approach and microdata to yield more accurate and robust insights compared to previous studies that relied on macroeconomic data. Particularly, the study employs data from the Danish National Patient Register, encompassing all elective and emergency hospital admissions and outpatient visits from 2000 to 2017. This extensive dataset provides detailed information on patient characteristics, including primary and secondary diagnoses coded using ICD-10 classifications. The authors leverage this dataset to conduct a repeated cross-sectional analysis of individuals experiencing health shocks, defined as emergency admissions indicative of significant changes in health status. The analysis stands out of previous macroeconomic studies, in that it controls for observable demographic and health drivers with greater accuracy. For instance, the study acknowledges potential influences from factors such as income elasticity and insurance coverage without assuming uniform impacts, allowing for a more nuanced understanding of the drivers behind HCE.
The research finds that the average HCE per person increased by 16.90% points in individuals experiencing an initial health shock in 2013-14 as compared to similar individuals in 2005-6. After controlling for variation in age, morbidity, and socioeconomic status, the increase in HCE between the 2 periods drops to 10.28% points, namely, the estimated RI of HCE that can be attributed to technological progress and change in medical practice. The RI accounts for about 60% of the total increment of HCE (i.e., 10.28/16.90 = 60.82%), whereas morbidity and age account for the remaining 40% (i.e., 1–10.19/16.90 = 39.70), with age only accounting for 7% of the total increment (i.e., 1–15.77/16.90 = 6.87). Socioeconomic status leaves the total increment unchanged.
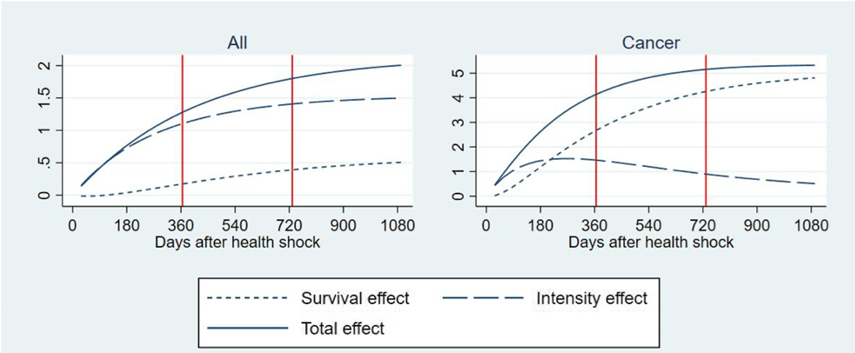
The authors conduct a heterogeneity analysis of RI by health conditions prompting the initial health shock, that is, the health condition reported as the primary diagnosis at the time of the health shock. When comparing cancer (colorectal, breast, prostate and lung) with all health shocks, there is a significant difference in how RI is decomposed. Figure 1 shows the RI of HCE (Y = 1000 €) in 2013-14 versus 2005-6 (baseline) decomposed into delaying TTD effect and intensity effect due to resource use. Figure 1 depicts the decomposition for all health shocks and for cancer. The cumulated total RI per cancer patient is two and a half times larger than for all health shocks amounting to a total of 5326 € 3 years after the shock. What is also very apparent is that the survival effect (i.e. the delaying TTD effect) is much more pronounced for cancer than for all health shocks.
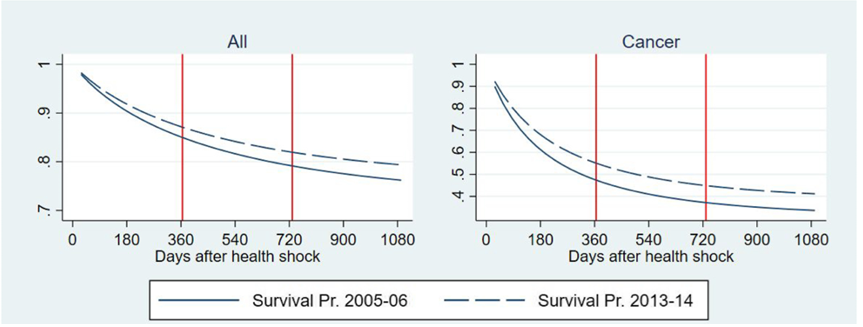
The large share of the RI due to the delaying TTD effect for cancer patients can be explained by a large improvement in survival outcomes (Figure 2) and a relatively small intensity of treatment effect in the average amount of resources allocated to patients after an initial shock due to cancer.
The methods presented in this paper offer valuable insights into cost drivers, that may explain the observed “steepening effect” and provide insights into how costs can be curbed. The findings carry substantial implications for health policy and resource allocation strategies. In the future, policymakers may need to balance the integration of new medical technologies with economic sustainability, while managing the increasing demand for healthcare services. This is particularly important in such countries as Italy, where recent reforms towards federalism – i.e. the attribution of more autonomy in policy making to regions – may undermine healthcare expenditure if this balance between new medical technologies and economic sustainability is not attained. Moreover, results challenge conventional beliefs that attribute rising healthcare costs exclusively to an aging population, advocating instead for a broader perspective that considers also technological contributions.

